You get the call from the hospital. The long-awaited and highly anticipated time is finally here; it’s the day you get your transplant and a new lease on life. What follows is likely to be a blur of going through checklists: do you have your go-bag? Did you notify your employer? Did anyone grab your favorite blanket? Who called the dog sitter? The last thing on your mind, if it’s even on your radar at all, is if the indoor environment you’re coming home to is safe. Now that we’re talking about it, did anyone during the pre-transplant process give you the lowdown on mold’s effect on transplant patient success?
Probably not…
This in and of itself is a bit baffling considering the amount of work doctors put into patients to ensure the transplant is a success.¹

They’ll assess the bloodwork, tissue samples, and crossmatch your antibodies against the donor to make sure the surgery will be a success. Then follows a series of progress monitoring after the surgery to make sure everything went well and your body is handling the new, foreign mass.
And then they send you home with a list of post-care instructions and a bag full of medication to suppress your immune system and make sure your body accepts the life-saving organ or stem cells.
Is where they’re sending you off to a safe environment to heal in, though? With recovery taking up to a year or more, it’s an important factor to consider. Since the medical community often neglects to discuss this aspect of successful recovery, it’s up to us, the public, to raise awareness and include indoor air quality in transplant post-op care.
Safety Doesn’t Stop at Hospitals
Sterilization is the name of the game for hospitals.² Medical professionals understand how important it is to make sure the indoor environments are as disinfected and free from contaminants as possible so that their patients have the absolute best odds for healing.
After the Covid-19 pandemic, many hospitals are going even further to ensure safe environments for their patients and taking a closer look at air quality.³ By installing better air filtration systems and using HEPA air filters, they’re attempting to remove as many foreign and harmful particles out of the air as possible for an extra layer of protection for patients.
This is a fantastic step in the right direction, as it helps remove particles such as mold spores. That’s right, hospitals are not immune to mold growth. They do an excellent job of disinfecting and sterilizing their indoor environments, but mold growth can happen anywhere, even inside the buildings dedicated to healing. For transplant patients, particularly, mold exposure can be especially detrimental. ⁴’⁵’⁶
Over the years, a few examples of mold’s effect on transplant patients have arisen. One instance occurred in 2015 at the University of Pittsburgh Medical Center.⁷ The medical facility suspended its transplant program following the deaths of three patients after successful transplant surgeries, with mold exposure as the culprit for such devastating outcomes.⁸ Since then, three other lawsuits have been brought against the hospital for mold-related deaths.

The basis of such lawsuits proves that mold exposure following transplant surgeries (or any surgery), can have catastrophic effects on patient recovery and can even result in death. This is why hospitals take such care to remove all contaminants and prevent situations in which environmental factors like mold from causing complications. ⁹
At this point, you’re probably thinking, "Fantastic! That sounds like great news for transplant success." And it is! That’s the first line of defense for successful recoveries. Typically, though, patients only spend 5-14 days in a hospital after transplant surgery. After that, the majority of healing occurs at home.
With a suppressed immune system, having an indoor environment that supports the healing process is paramount.
Why Are Transplant Patients At Risk?
After the first successful organ transplant in 1954 (it was a kidney for those curious!), there have been a number of medical advancements to ensure that the patient’s body does not reject the foreign object. ¹⁰ One such example is immunosuppressants.
While the body needs these new organs or stem cells to get back on track and keep an individual alive and well, it does not take kindly to things it thinks don’t belong. ¹¹ Similar to a pet assuming anything new brought inside a home is public enemy number one. The body’s immune system will focus on this foreign entity, consider it a threat, and wage war on it until it’s removed from the body.

Any other time that’s fantastic for us, like in the case of viruses and bacteria. Battle away, rockstar immune systems! When it comes to a new heart that’s needed for survival, that’s when the thoroughness of the immune system is a problem. This defensive system in the body will create cells and antibodies that will attack and damage the new heart, causing the body to reject the organ. With a stem cell transplant, the new and improved immune system will consider the entire body an enemy and attack healthy cells and tissues.
Hence, why immunosuppressants were created to control and suppress this automatic immune system response. That way, the body has time to adapt to the new addition.
It’s important to create a healthy environment to heal for any patient after surgery. When it comes to transplant patients, in particular, this is even more crucial because of their scheduled and prolonged regime of immunosuppressants.
Often taken for the entirety of that transplanted organ’s life within the body. The dosage is lowered over time, and researchers are hard at work attempting to find an alternate method for success so patients don’t continually have to take these drugs, but those individuals taking the medication do not have a fully charged and operational immune system. ¹²’¹³
This situation can open the door for adverse health events, such as reactions to opportunistic particles. Especially in the beginning when the immunosuppressant doses are turned way up. That’s why doctors harp on staying away from any possible contamination areas, continually washing hands, and disinfecting surfaces as much as possible. They don’t always cover every threat though. Some negative health reactions can be triggered by mold.¹⁴ That’s why mold’s effect on transplant patients needs to be considered and plans set in place preemptively to mitigate exposure.
So What Is Mold?
Before we touch on what should be added to the protocol for transplant patients, it’s best to know what these individuals’ bodies could be battling against.
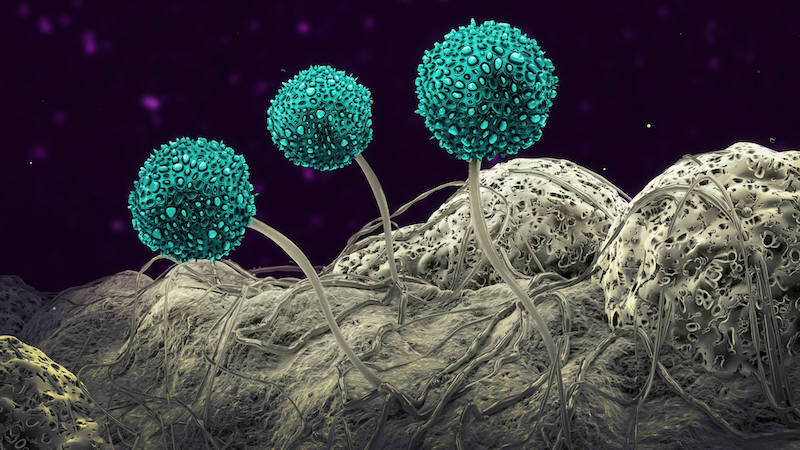
Mold is a type of fungus with over 100,000 species identified so far.¹⁵ They reproduce by creating microscopic spores, similar to the seeds released by a weed. These tiny, invisible seeds then ride the air current wherever that may take them: inside your car, onto your clothing, and right through the front door of your home. ¹⁶
All of which isn’t a problem. Mold is a necessary and important part of nature. The issue begins when this tenacious fungus starts growing inside of your home. Once it finds a comfy and habitable location, it will put down roots and release more and more spores into the air. What constitutes a great moldy home? Four simple factors:¹⁷
- Oxygen (they require very little)
- Food (they eat almost anything)
- Temperature (a temperature-controlled indoor space is a mold spore’s dream)
- Moisture (the key ingredient)
Provide spores with a damp space for 24-48 hours and they’ll be in heaven. The new spores that are released can then opportunistically colonize other areas of your home (leading to even more spores). But, more importantly, indoor mold growth immediately begins affecting the air quality of your home. All of those spores are trapped within the confines of those walls.
Poor air quality can wreak havoc on anyone’s health, and that’s not even considering how mold affects transplant patients’ health and the issues it can cause.
Mold’s Effect on Transplant Patients (And General Health)
Researchers are hard at work attempting to determine exactly how mold exposure affects our health. With over 100,000 species and the relationship between genetics and preexisting conditions, it’s a tough subject to nail down. Some individuals are just innately more susceptible to experiencing symptoms faster and more severely than others due to a combination of those factors. ¹⁸’¹⁹
What researchers do agree on is that those with developing or compromised immune systems are more at risk for developing symptoms.²⁰ Who has compromised immune systems? Transplant patients who are required to take an immunosuppressant drug cocktail.
To make matters even trickier, some species of mold also have the ability to create microscopic toxins, called mycotoxins.²¹ These particles can also, you guessed it, have detrimental effects on health. Not to mention, if mold growth exists in a home due to a large water event, it’s not just mold and its byproducts we have to worry about. Bacteria, another harmful microscopic organism, may be present to further affect our wellbeing.
In short, it’s an air quality and health nightmare, particularly for individuals with a downed internal protection system.
Typically, mold exposure can cause symptoms ranging from mildly irritating to severe. These include:
- Brain fog
- Chronic Fatigue
- Headaches
- Respiratory Issues
- Digestive Problems
- Neurological Issues

For those who have had post-transplant surgeries, the results of mold exposure can be far more detrimental. Studies abound detailing the effects this fungus can have on transplant recipients post-surgery. From infections and respiratory issues to prolonged healing and even death, mold can cause a devastating blow to these immunosuppressed and healing individuals. You can check out the links below for a list of some of these studies.
Hospitals are hard at work making sure that this exposure doesn’t happen in their facilities, but what about after that? What’s preventing exposure in the place patients spend the majority of healing: their own home?
With how easily mold growth can occur coupled with the blur that is pre-transplant surgery, it’s very easy for homes to be culprits for a slew of adverse reactions in recovering patients.
Avoiding Mold’s Effect on Transplant Patients
Transplants are often critical for patient survival and to help them live their lives to the fullest. It’s one of the amazing additions provided by modern medical advancements. However, post-care doesn’t just extend to follow-up appointments, eating properly, following medicine guidelines, and sticking to healing protocol timelines.
Even though it’s an undiscussed topic, transplant patients need to ensure their homes are also free from mold growth and filled with clean, healthy air quality. When you consider that the average person takes over 20,000 breaths a day, transplant patients are at home for a good portion of their recovery, and immunosuppressants are required for a good, long while, it’s easy to see why removing contaminants that can drastically impact health is critical. ²²
There were over 39,000 transplants performed in the United States alone in 2020.²³ How many of those recipients were briefed on the dangers of mold and provided direction on how to prevent and avoid exposure? More than likely, not enough. Even with the number of studies pointing to this silent and often invisible threat.
Until creating a safe home environment is a standard part of transplant protocol, it’s up to the patients and support systems to ensure homes are the safe environments needed for healing. The following steps are important pieces to include in the recovery protocol.

Testing
First and foremost, those who are on track for an organ or stem cell transplant should test the air quality in their home. Early detection of a problem can help prevent any exposures after the surgery and the immunosuppressant drugs take effect. Keep in mind, it’s not just mold that may be present and can negatively impact transplant patients. Other indoor contaminants like asbestos, mycotoxins, bacteria, and other particulate matter can also be a problem. ²⁴
Hiring someone to come in and test the air quality inside the home can give you a snapshot of the indoor air quality and any contaminants that may be present. Knowing about them beforehand will allow time for corrective action to be taken to minimize these issues so that they don’t interfere with recovery.
Not all air quality professionals are the same, though! Those who assess mold, in particular. When you hire an individual, make sure that they understand the situation and have the patient’s health as the utmost priority.

The inspection itself should cover the entire home, take a few hours, and use a variety of measuring techniques. There’s not a one-measurement-detects-all-contaminants method as of yet, so thoroughness is key to ruling out as many issues as possible.
Some of the testing data you should expect to see includes:
- Types of molds present
- Quantities of each mold
- Potential spore presence in the HVAC system
- Presence of mycotoxins (a harmful toxin produced by molds)
- Presence of bacteria
The more data, the better. From there, you’ll be able to tell if there are problem areas that need to be dealt with prior to the surgery. Consult a trusted professional who understands the importance of creating a clean indoor space to take a look at the results and point out any potential problems that need to be addressed.
Remediation
If the data shows a mold and contamination problem, getting rid of the problem should be tackled as soon as possible.
Like air quality inspectors, not all remediation companies are created equal. You need a team that hangs their hat on creating a healthy indoor space and understands how crucial it is to deal with a mold problem correctly. They should 100% understand mold’s effect on transplant patients and how important their job is. Otherwise, colonization in the house could still exist in other areas that weren’t treated, the mold could return, or byproducts like mycotoxins could be left behind.
The company you choose to work with should use the data collected as a roadmap to thoroughly and properly remediate the home. They should be equipped to deal with the entire scope of work so that when they leave, you’re left with a safe indoor space that is prime for recovery.
This team should stand on three pillars for a successful remediation protocol:
- Remediate the sources properly.
- Identify and address what led to those sources in the first place.
- Eradicate all contamination created by these sources.

By leaving any of these steps out of the protocol, the remediation won’t be considered a success. Neglected areas like hidden mold in a wall will still contribute to exposure. Mycotoxins left behind (because they have to be removed differently than mold) will still trigger adverse health reactions. Not fixing the source of a water event that led to mold will just lead to more mold growth down the road while the transplant patient is taking immunosuppressants.
Every little piece in a remediation protocol is connected and important for the successful treatment of a home, and for the health of those that are inside.
Prevention
If the air quality results came back positive, that’s fantastic! That’s one completed checkmark needed for a successful recovery. Mold and air quality awareness doesn’t stop there, though.
While the transplant recipient is in the hospital, a careful eye needs to be kept on the house to make sure no water events occur and that preventative actions continue to discourage mold growth inside. From there, similar action needs to be taken once the patient gets home and continues the recovery process. That way, mold’s effect on transplant patients can be avoided as much as possible.

Preventative actions to avoid mold growth include:
- Ensuring that the HVAC system is in good working order and is a good fit for the home.
- Installing air purification systems (just for added protection)
- Addressing leaks immediately
- Maintaining indoor humidity between 30-50 degrees ²⁵
- Regularly cleaning with EPA-approved cleaning products that properly deal with mold particles and byproducts
- Checking hidden areas prone for water events, like the basement, attic, and crawl space
- Creating and maintaining better ventilation within the home (like turning on the bathroom exhaust fan while showering)
Preventative steps taken now can help avoid any issues down the road. Again, immunosuppressants will be there for the long haul, which means safe indoor environments are an extra point of concern and an area to pay attention to. Plus, avoiding remediation can help save money, which is never a bad thing after the medical bills following surgery.
Creating Awareness of Mold’s Effect on Transplant Patients
In total honesty, there’s no good reason why mold awareness isn’t included in the discussion regarding transplant recovery. With how drastic mold’s effect on transplant patients can be, it should be among the top factors to pay attention to while healing.
It’s up to us, whether patients, support systems, or concerned individuals, to raise awareness of the need to create healthy indoor spaces for those recovering from surgery. No one should have to go through surgery, all the medical costs associated with care, and the long and trying days of recovery just to fall victim to an unseen threat: mold exposure. Recognizing the potential problem and actively taking steps to stop its effect can do a world of good towards eliminating it as a threat for transplant patients.
While it may seem like an added stressor at first, on top of the long list of things required for successful recovery, it’s no less important. When in doubt, contact an expert who can help you prepare and answer any questions you may have. Not only will it give you peace of mind, but it will also help create the foundation necessary for recovery so transplant patients can begin the next, and most important, chapter: enjoying life with a healthy body.
For More Information of Scientific Studies Click On The Links Below:
- Invasive mold infections in solid organ transplant recipients.
- Mold Infections in Solid Organ Transplant Recipients.
- IL1B and DEFB1 Polymorphisms Increase Susceptibility to Invasive Mold Infection After Solid-Organ Transplantation.
- Fungi and molds following lung transplantation.
- Invasive non-Aspergillus mold infections in transplant recipients, United States, 2001-2006.
- PTX3 Polymorphisms and Invasive Mold Infections After Solid Organ Transplant.
- Invasive fungal infections in transplant recipients.
- Epidemiology, outcomes, and mortality predictors of invasive mold infections among transplant recipients: a 10-year, single-center experience.
- Antifungal prophylaxis among allogeneic hematopoietic stem cell transplant recipients: current issues and new agents.
Citations:
- CDC. (2019, January 18). Transplant Safety. Centers for Disease Control and Prevention. Retrieved October 28, 2021, from https://www.cdc.gov/transplantsafety/index.html.
- Boyce, J. M. (2016). Modern technologies for improving cleaning and disinfection of environmental surfaces in hospitals. Antimicrobial Resistance & Infection Control, 5(1), 1-10.
- Mousavi, E. S., Kananizadeh, N., Martinello, R. A., & Sherman, J. D. (2020). COVID-19 outbreak and hospital air quality: a systematic review of evidence on air filtration and recirculation. Environmental science & technology, 55(7), 4134-4147.
- Husain, S., Alexander, B. D., Munoz, P., Avery, R. K., Houston, S., Pruett, T., ... & Singh, N. (2003). Opportunistic mycelial fungal infections in organ transplant recipients: emerging importance of non-Aspergillus mycelial fungi. Clinical Infectious Diseases, 37(2), 221-229.
- Kauffman, C. A. (2006). Fungal infections. Proceedings of the American Thoracic Society, 3(1), 35-40.
- Asim A Jani, M. D. (2021, October 16). Infections After Solid Organ Transplantation. Medscape. Retrieved October 28, 2021, from https://emedicine.medscape.com/article/430550-overview.
- Yan, H., & Brumfield, B. (2015, September 22). Pittsburgh hospital suspends organ transplants after mold infections, deaths. CNN Health. Retrieved October 28, 2021, from https://www.cnn.com/2015/09/22/health/pittsburgh-organ-transplant-deaths-mold-fungus/index.html.
- Howard, D. (2015, September 26). The same types of mold that shut down the Umpc transplant program could be in your home. House to Home. Retrieved October 28, 2021.
- CDC. (2020, August 4). About Healthcare-associated mold outbreaks. Centers for Disease Control and Prevention. Retrieved October 28, 2021, from https://www.cdc.gov/fungal/outbreaks/healthcare-associated-mold-outbreaks.html.
- UNOS. (2021, June 3). The history of organ donation and transplantation. UNOS. Retrieved October 28, 2021, from https://unos.org/transplant/history/
- Cleveland Clinic , M. P. (2021, March 17). Immunosuppressants: Definition, treatment & what is it. Cleveland Clinic. Retrieved October 28, 2021, from https://my.clevelandclinic.org/health/drugs/10418-immunosuppressants.
- Hsu, D. C., & Katelaris, C. H. (2009). Long-term management of patients taking immunosuppressive drugs.
- Cohen, S. (2021, August 4). Transplants minus a lifelong regimen of anti-rejection drugs? it's becoming a reality at UCLA health. UCLA Health. Retrieved October 28, 2021, from https://connect.uclahealth.org/2021/08/04/making-transplants-without-a-lifelong-regimen-of-anti-rejection-drugs-a-reality-at-ucla-health/.
- CDC. (2020, December 17). Organ transplant patients and fungal infections. Centers for Disease Control and Prevention. Retrieved October 28, 2021, from https://www.cdc.gov/fungal/infections/organ-transplant.html.
- Environmental Protection Agency. (n.d.). Mold. EPA. Retrieved August 17, 2021, from https://www.epa.gov/mold.
- Centers for Disease Control and Prevention. (2020, August 11). Basic facts about mold and dampness. Centers for Disease Control and Prevention. Retrieved August 17, 2021, from https://www.cdc.gov/mold/faqs.htm.
- Lstiburek, J., Brennan, T., & Yost, N. (2002, January 15). Rr-0208: What you need to know about mold. Building Science Corporation. Retrieved August 18, 2021, from https://www.buildingscience.com/documents/reports/rr-0208-what-you-need-to-know-about-mold/view.
- Curtis, L., Lieberman, A., Stark, M., Rea, W., & Vetter, M. (2004). Adverse health effects of indoor molds. Journal of Nutritional & Environmental Medicine, 14(3), 261-274.
- Bush, R. K., Portnoy, J. M., Saxon, A., Terr, A. I., & Wood, R. A. (2006). The medical effects of mold exposure. Journal of Allergy and Clinical Immunology, 117(2), 326-333
- Environmental and Occupational Health Assessment Program, & Environmental and Occupational Health Assessment Program, & Health Science Section, Mold Basics for Primary Care Clinicians (2009). Hartford, CT; Connecticut Department of Public Health. , H. S. S., Mold Basics for Primary Care Clinicians 1–10 (2009). Hartford, CT; Connecticut Department of Public Health.
- World Health Organization. (n.d.). Mycotoxins. World Health Organization. Retrieved August 26, 2021, from https://www.who.int/news-room/fact-sheets/detail/mycotoxins.
- Brown, A. (2014, April 28). How Many Breaths Do You Take Each Day? [web log]. Retrieved October 8, 2021, from How Many Breaths Do You Take Each Day?
- UNOS. (2021, August 6). Organ transplant trends: More transplants than ever. UNOS. Retrieved October 28, 2021, from https://unos.org/data/transplant-trends/
- Howard, D. (n.d.). Organ transplant patients are at risk for mold exposure in the home. mold exposure can be deadly to these and other immuno-suppressed patients. Home Pittsburgh Area Mold & Environmental Testing, Inspection and Consulting. Retrieved October 28, 2021, from http://homeinspectionsbydanhoward3.proiwebsites.com/OrganTransplant.
- EPA. (n.d.). A Brief Guide to Mold, Moisture and Your Home. EPA. Retrieved October 26, 2021, from https://www.epa.gov/mold/brief-guide-mold-moisture-and-your-home#tab-6.

